In the presence of colorectal and anus diseases, it is necessary to consult a haemorrhoids specialist. In this article, you will find out who the proctologist is and what he does; what a proctological examination consists of; what are the most frequent pathologies and how they are treated; when the haemorrhoids specialist responsibility exists.
You have been experiencing strange symptoms such as cramps and abdominal pain for some time, yet you have not done any kind of physical exercise. Yours is a pang to which you can not give an explanation. You also have some nausea, constipation and diarrhea. Or maybe you have prolonged and persistent anal pain. You may have found blood in your stool. In short, you are struggling with annoying disorders or disorders of the colon and anus. Who can you contact in these cases? To the proctologist.
Who is he and what does he do? He is a doctor who deals with diseases affecting the colorectal system and the anus. The etymology of the word “proctology” comes from the Greek “procto” (anus) and “logia” (speech).
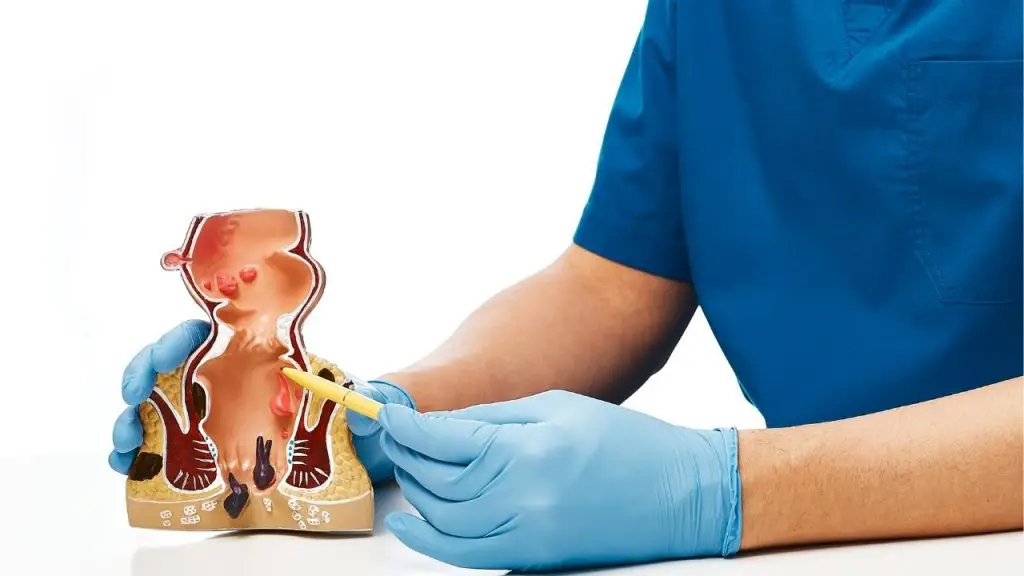
What does the proctological examination consist of? In a rectal examination, performed by the proctologist, associated with an instrumental investigation, the anoscopy, performed with the anoscope.
What are the pathologies treated by the proctologist in detail? Hemorrhoids; anal fissures; rectal prolapse; polyps; Crohn’s disease; anal fistulas; anal warts; diverticula; irritable bowel syndrome. If you want to know more about the symptoms, causes and treatments of these diseases, continue reading my article. Here, you will find the interview with dr. Giorgio Falcetto, specialist in general surgery and vascular surgery. After that, I will tell you about the responsibility of the surgeon.
Haemorrhoids specialist, what’s its name, and what does he do?
The haemorrhoids specialist is commonly known as proctologist. The proctologist is a surgeon who is interested in ano-perianal disorders and colon disorders. Often, he has to deal partly with the anterior sphere of the perineum.
Examination by the haemorrhoids specialist: what is it and when is it necessary?
It is a visit that, in general, is aimed at ano-perianal disorders, most often related to hemorrhoids, fissures, rarely to fistulas. Sometimes, hemorrhoid prolapse or even intestinal prolapse; to perianal abscesses or to the outcomes of abscesses which are perianal fistulas.
The proctological examination by teh haemorrhoids specialist is always completed with anoscopy which consists of an inspection with an instrument (generally, disposable) of the anal canal, made with the appropriate lighting that gives us news not only of the anal canal, but also of the ampoule rectal which is the area of the anus where the faeces stop before coming out. Sometimes, this area is prone to inflammation and infection.
How to prepare for the proctological examination?
Generally, the proctological examination does not require preparation.
Proctological examination: what is it for and what does it consist of?
The first approach is an inspection to look at the anus and the skin around the anus which is sometimes subject to mycosis. In this case, the skin is very red. The cause of mycosis is often linked to excessive hygiene. Therefore, by using soaps on soaps, the natural protections of the anus are removed and the fungi that cause mycosis end up prevailing, which will then be treated with the appropriate creams.
The second step of the proctological examination is the exploration with the finger that allows us to feel what the sphincter tone is, therefore to understand if the anus has a good contractility or a tendency to have a release of tone that facilitates prolapses or, even, an increase in tone when there is inflammation. For example, in the case of fissures there is an increase in tone, as a result of which the exploratory finger is contracted by the circular mucosa of the anus.
The exploration concerns the inside of the anus and the rectal ampoule and allows you to perceive and palpate the possible presence of masses that may be tumors or simple polyps. In addition, it allows us to check whether there is bleeding in the rectal ampoule, when the finger is removed.
In men, the exploratory finger inside the anus, in the front part, feels the prostate and also highlights if there are infections there (it is not a neurological examination). In women, the cervix is felt which, however, is easier to explore vaginally.
After the exploration with the finger, the anoscopy is done, with a rigid instrument we were talking about before, which is introduced into the anal canal for about ten centimeters, it allows us to check whether in the anal canal, and just below it, there is they are inflamed fissures or hemorrhoids. It also allows us to see if the mucous membrane of the rectal ampulla is inflamed and thus an infection called proctitis is configured, which often has bleeding and irritation.
In which cases is rectoscopy required?
Rectoscopy is an examination done with a rigid instrument of 25 cm, no more than 8-10 cm like the anoscope. It is a more traumatic examination that allows us to have information on the last 25 cm of the rectum. In this case, a certain preparation is required to perform the rectoscopy, that is to say, the patient must have cleaned the last part of the intestine with care or enemas to give the person performing it the opportunity to see the walls of the intestine well. rectum and sigmoid.
Nowadays, rectoscopy is hardly used anymore, because it provides us with limited information and, in addition, it is a bit painful. Rectoscopy is sometimes adopted by the surgeon after surgery.
The rectoscopy was replaced by a colonoscopy.
What is colonoscopy used for?
Colonoscopy gives us information on the whole colon up to the ileocecal valve which allows us to be operative because with colonoscopy, if there are polyps, they can be removed or biopsies to verify the nature of the polyp itself. With colonoscopy it is possible to highlight in the various segments of the colon if there are any inflamed tracts.
What is the duration of the visit by the haemorrhoids specialist?
In about 10 minutes, the proctological examination is over.
Is the proctological examination painful?
It depends on the pathology. If it is an anal fissure, the rectal examination alone is very painful. In the case of anal fissure, anoscopy is not done precisely because the patient feels pain already upon the introduction of the exploratory finger, let’s imagine at the introduction of the anoscope. Even in the case of hemorrhoids, the examination is painful on palpation of thrombosed hemorrhoids alone. In the other cases, with a good collaboration of the patient who tends to relax and relax the sphincter, the proctological examination is not painful.
Hemorrhoids: what are the symptoms, causes and remedies?
Among the most frequent causes, we find stress which causes an increase in the tone of the sphincters and inflammation of the hemorrhoids.
Hemorrhoids are painful if they are thrombosed, that is, if the blood that has reached the hemorrhoids stops and cannot flow. In this case, we are talking about subcutaneous, external hemorrhoids that are the size of a hazelnut. They are very painful to the touch and prevent the patient from sitting down. Subcutaneous hemorrhoids must be differentiated from internal hemorrhoids which are located inside the anal canal, in an area defined as “toothed” and are those that bleed. Internal hemorrhoids are those that tend to slide outwards and do not return after defecation. On the other hand, subcutaneous hemorrhoids give considerable pain if they thrombus, coagulated blood is formed that is not reabsorbed.
In the case of external thrombosed hemorrhoids, therapy is immediate, because local anesthesia is enough to cut the skin covering this thrombus, so the clot comes out and the patient is immediately well. In this case, a small surgery is decisive and, in a short time, the patient is free from his pathology.
As for internal hemorrhoids that prolapse outwards, however, anti-inflammatory creams or preparations must be used. If after defecation or with the help of the visit, they automatically re-enter the anal canal, they can then be treated surgically or with outpatient treatments which are elastic ligation and cryotherapy.
Cryotherapy allows us to freeze hemorrhoids internally, below that famous dentate line that is the “pain line”: we can freeze everything above it, while what lies below (such as subcutaneous hemorrhoids) needs of anesthesia and, in those cases, neither elastic ligation nor cryotherapy should be used.
Anal fissures: what are they?
Cracks are also a pathology linked to tension; they are due to a small cut. There are fissures related to a more systemic pathology such as Crohn’s disease, but these are not painful fissures. The common fissures we are talking about are small cuts that form in the anal canal below the mucosa up to the internal sphincter muscle causing a spasm and that is what causes the fissure pain. The fissure bleeds and the spasm is painful.
Anal fissures: how are they treated?
Treatments for fissures are based on the use of creams that have an antispasmodic function, because they are based on nitrates. There are various types of creams with nitrate concentrations from 30% to 70%.
If this type of treatment does not work, anal dilators can be used to remove the spasm and dilate the anus so that the fissure has a chance to heal. They are applied for half an hour for three evenings, they are lubricated and kept in place to determine muscle relaxation and to promote the healing of fissures.
If this type of treatment fails, then we move on to surgery that does not involve the anal canal, but works externally. Local anesthesia is done laterally, outside the anus, to see which is the internal sphincter muscle and which are the fibers. Some fibers are blown up. This operation must be done in a very adequate way by those who habitually practice it to avoid damage. The operation does not touch the anal canal and is decisive.

Anal warts: what are they?
They are sexually transmitted diseases, related to anal intercourse. They are growths of flesh that are easily highlighted on the outside of the anus; if left in place, they continue to increase. They are not painful. Condylomas can be limited to the external part, to the skin of the anus and perianus. However, they can also be internal, because in anal intercourse they are brought by the member inside the canal. They can be seen through anoscopy.
Anal warts: what are the symptoms?
Condylomas have no symptoms. The patient on the outside sees them, he can perceive them and if he looks in the mirror he can also see them. Clearly, he cannot see those who are inside. Rarely, one of the symptoms that can occur in the case of internal warts is bleeding and this is what then leads the patient to consult the proctologist.
Anal warts: how are they treated?
For the treatment, you can start with creams that favor its destruction. The most common treatment is the laser. After the condylomial treatment, checkups are made for three to six weeks to see that there are no relapses which, in case, must be treated immediately.
Rectal prolapse: what is it and what does it involve?
We need to make a difference between hemorrhoid prolapse and rectal prolapse. Prolapse of hemorrhoids is very common and resolves with the manual re-entry of the hemorrhoids into the anal canal and can be treated with cryosurgery.
Rectal prolapse is the sliding of the mucous membrane of the rectal ampulla and into the last piece of the rectum outside the anal canal. This prolapse is disabling, often the piece of intestine comes out without the need to evacuate. This leaked piece of intestine soils the undergarments with serum and sometimes with blood.
Rectal prolapse: how is it treated?
In the most important cases, rectal prolapse must be treated surgically. Through the surgical operation, the intestine is repositioned by pulling it from above, bringing it back into the abdominal cavity and fixing it. This operation was previously done in open surgery, while today it can be done in laparoscopic surgery. The patient goes to sleep and to avoid a new sliding outside the intestine is fixed to the sacrum. In these cases, the sphincter of the anal canal must be fairly toned, otherwise there is a recurrence.
Another operation that is done in the case of rectal prolapse is the cerclage of the anal canal. Spinal anesthesia is performed and a “bandage” is placed under the skin in parallel with the sphincter. The bandarella must be well adjusted, because if it is too wide it is useless, if it is too narrow there is difficulty in defecation. The bandarella is rigid, not elastic.
Responsibilities of the haemorrhoids specialist: guidelines and good medical practices
After analyzing the pathologies that the haemorrhoids specialist deals with, we can now talk about the responsibility of the surgeon.
Let’s assume that in the treatment of rectal prolapse or anal fissures, the surgeon has performed the surgery incorrectly and has not adopted the necessary precautions or good clinical care practices, thus causing serious harm to the patient, as well as great pain. Will the doctor answer for the injuries caused to the patient?
According to the law, the physician is criminally responsible who in the event of health inexperience, incompetence, negligence or imprudence has not respected the guidelines or good medical practices (interventions, strategies and approaches aimed at preventing unexpected consequences and improving the safety level of health care).
So, in which cases does the doctor not respond criminally? Everything revolves around the concept of observance and adoption of guidelines and good medical practices. If the doctor has adapted to them, he will not be able to respond criminally for the fact, unless he has adopted guidelines that are inadequate for the specific case, that is, those provided for a pathology other than that from which the patient suffers.